An Interview with Psychologist Larry Rosen
Dr. Rosen is past Chair and Professor Emeritus of Psychology at California State University. He is a research psychologist and recognized as an international expert in the psychology of technology. Upon his diagnosis of Parkinson’s Disease, Larry Rosen has sought to educate, mentor and guide others utilizing both a humanistic and scientific approach.
Jennifer Ghahari: Hey, thanks for joining us today! I'm Dr. Jennifer Ghahari, research director at Seattle Anxiety Specialists. I'd like to welcome with us Psychologist Larry Rosen. Dr. Rosen is past chair and professor emeritus of psychology at California State University. He is a research psychologist and recognized as an international expert in the psychology of technology.
He has given keynote speeches to Fortune 500 companies and nonprofit organizations in the US and internationally. Larry has been featured extensively in national television, print, and radio media. Before we get started today, can you let our listeners know a little bit more about you as well as your current research endeavors?
Larry Rosen: Sure. Thanks for having me, and I'm looking forward to chatting with you. I've been studying what I now call the psychology of technology since the early 1980s when there were no laptops, no smartphones, no nothing. You wanted to use the computer, you punched cards. You handed them to somebody who went into a very cold room, and they ran them. If you were lucky, you got to print-out this thick. If you weren't, you got a print-out that thin, and it meant there was an error, and you had to do it all over again.
What I was interested in way back then was something called computer phobia. And this is when computers were coming out. People were trying to use them. People were a little scared of them, a little frightened, a little weirded by them. Then we just kept changing what we were studying as life changed.
So, we went from computer phobia to technophobia, and we then went to tech and stress. Back I can't remember how long ago, I wrote a book called TechnoStress, which is funny because I reread it the other day. Most of what we said in my book was true, and yet it's probably 15 years old, if not more. We were looking at TechnoStress that you had at work, at home, and at play. So, it was invading everything.
Jennifer Ghahari: Oh, wow.
Larry Rosen: Then, since then, I've just kind of gone with the flow, whatever's interesting. I always tell people that whatever my kids are doing and my grandkids are doing is what I want to study.
Jennifer Ghahari: Nice.
Larry Rosen: I have a very low boredom threshold. So I'll study something for a while, and then I'll think I've got it. Then I'll move on and study something else. So I have worked my way to what I'm working on now. By the way, I'm retired, although retired just means I'm retired from teaching. I still do research, and I'm still very active on boards of directors for a lot of these groups.
One of the areas that I'm very interested in, I can only do this now that we've got newer technology, is what are people doing on their smartphones. As a corollary to that, what are teenagers doing? What are millennials doing? What are adults doing? We haven't really had the tools to do this until now, really till the iPhone got screen time and Android got digital wellbeing, I think they call it.
We were able to actually in the background have something track what people are doing, and what we get is an assortment of really valuable information. What I've done is had groups of teenagers and millennials at the end of their week when it pops up on screen time and says, "You've used 18 hours a day this week," or whatever the hour is, and then they can go back and get seven days' worth of data.
Because Apple doesn't allow them to download it, they take screenshots, they send us the screenshots. We then analyze them. What we're able to get from screen time is really quite a good picture of what people are doing. First of all, we get the gross amount of hours per week, hours per day. That sometimes can be telling if they're spending a lot, a lot of time on, particularly kids, perhaps video gamers, a variety of people who spend time on their phone.
We also get information on what apps they spent most time on. We get information on when they unlock their phone... Whether they have a face ID or a number ID or whatever or none, when they unlock their phone, what is the first app they tap? We also get how many times a day they unlock their phone, and we also get how many notifications they got each day and where they came from.
So, you can imagine we're compiling this set of data to be able to look at what everybody's doing out there because it's very clear. People are on their phones all the time. I mean, that's undeniable. I can't tell you how many times during the day I'll be at a stoplight, and there'll be a car in front of me. Light will turn green and be waiting and waiting. Oh, yeah. They're looking at their phone. Honk. "Oh, yeah. Sorry. I'll move on."
We take those 45 seconds and think we have to do something. We have to look at our phones, and we have to keep up. Otherwise, we think we're missing out on something, which is, by the way, why FOMO, fear of missing out, has developed because we have this sense that we're missing out on something.
Another attack that we tried to do, which, by the way, was a dismal failure, was to see if we could give teens and millennials strategies of how to treat their phone in a way that they might use less time on their phone. They might pick it up less often. We first tried giving them all sorts of choices. Some of them were take your icons for your social medias, put them in folders, scatter the folders all over the place so you don't know where they are thinking, "Well, they have to keep scrolling, and find the folders, and put the folders inside the folders, and whatever." That didn't work.
We tried to teach them how to meditate in order to be a little more calm when they approached their phone. That didn't work. We tried to teach them how to integrate technology into their work, such that instead of taking work breaks, they were taking tech breaks. That didn't work. I won't say it didn't work. It worked for the three weeks that we did it, and then as soon as we stopped, they went right back to where they were before. So then we tried it with fewer choices, but six weeks, and the same exact thing happened. They just went right back to where they were.
So, who's to blame for this? Because that's really what people are asking us. Who do we blame? Where do we point the finger at people who can maybe make changes? Obviously, one place to point your finger is at yourself. I think that's the first choice is you got here yourself. You didn't just stumble on it. You developed this habit, this way of treating your phone and in such a way that even if your phone is not in your pocket and you feel a little itch down there, you think that your phone is vibrating, which by the way is called pocket vibration syndrome, and is real. We experience it all the time.
The other thing we noticed is that when people walk around, say, from class to class at a campus or just walking around the campus, they are always carrying their phone in their hand because it is close. There is a point where women, girls used to put it in their bra, tuck it in there so that they really felt that vibration immediately, and then take a look, and see who's there.
Jennifer Ghahari: Wow.
Larry Rosen: The feeling is... It's when someone beckons you, whether it's instant message or whatever. When they beckon you, you feel compelled to go. I use that word, compelled, as part of the phrase, OCD, obsessive-compulsive, compelled, compulsive, behavior because a lot of what's going on is we are acting based on anxiety.
What are we anxious about? Well, we're anxious about missing out on things. We're anxious about not being Johnny on the spot when somebody texts you and texting them right back. We're anxious about a lot of things that take place on our device. Usually, it's the smartphone. Some people, it's the iPad, but in general, it's a smartphone, and in general, it's an iPhone. I will use iPhone as the whole generic category of Android and all those.
What we find is that we have lost control. What I mean by losing control is that we really don't understand why we're doing what we're doing. We just feel compelled, and that's the anxiety part. For example, take a typical teenager. They unlock their phone. They tap on an icon. We even have them take a picture of what icons are on the front screen. They're almost all the connection, text messaging, other kinds of messaging, instant messaging, lots of icons for social media. They're all there. They're all sitting there, waiting.
So, of course, you open your phone, the first thing you do is tap. The one you tap first may very well be the one you use the most, or it's the one that stands out the most, or it's the one that notified you. We have a compulsion to do that because if we don't, then chemicals in our brain and body start to build up and make us more, and more, and more anxious. So when we can't do it, we get anxious.
One of my colleagues, Dr. Nancy Cheever, did a really interesting study. You can actually see the study in action. If you go on my website and look at the very top where it says, "Anderson Cooper. Watch Anderson Cooper on 60 Minutes." So Anderson Cooper came into our lab and, Jenn, really nice guy. Came into our lab. Nancy sat him down at a desktop and said, "Okay, what we're going to do is show you a video and have you answer some questions later. We just want to put a couple of little things on your fingers," which now most people recognize one's an oximeter. Because of COVID, they know that.
The other one is more important. It's called galvanic skin response, which is the sweat on your skin. The sweat on your skin is equated to arousal, and arousal can be either positive arousal or a negative arousal. I mean, if I'm going to give a speech, my hands get very sweaty. It's not that I'm anxious about it. It's I'm excited. I'm excited to do it. But if I'm facing a really difficult thing that I have to do that's very uncomfortable, my hands might sweat, and that's anxiety.
So told Anderson, "Just put your phone upside down next to you," and then Dr. Cheever gave him about a minute or so of starting. She said, "Wait, wait, wait. We have to stop. That phone that you put down to the side is interacting with the two little clips, and so we're just going to need to move it behind you." She put it on a table behind him, and then she started texting him, but he could not answer.
She texted him four times. Every single time, galvanic skin response... spikes.... spikes... spikes four times in a row. We've done this with a lot of people, famous people, news, media, whatever. The interesting thing is it's always the same, except for one case, and I'll tell you the one case. What Anderson Cooper told us very clearly is, yeah, as soon as that beep went off, he felt a little rush in his body, which is galvanic skin response, and he felt like he was missing out on something, and he had to-
Jennifer Ghahari: Wow.
Larry Rosen: He felt like he had to check it right now, but he couldn't because we wouldn't let them. Now, interesting enough, people have very different ideas of why they need to check it. couldn't because we wouldn't let him now. Katie Couric, for example, felt like when her daughter was texting, she needed to pick it up quicker.
Steve Aoki, who I don't know if you know who he is, but he's a very famous DJ, and he travels with an army of people, all who monitor his social media, so he showed nothing because he didn't need to. His social media was being monitored by all of his team, and so he didn't show anything.
Two teenage girls, however, were brought in, and they showed not just spikes, but spikes. It was like, "Oh my God. What am I missing out on?" Part of it is because you know that if you get a text, for example, from someone, and you don't respond immediately, they'll text you back and say, "Are you mad at me," or, "Why aren't you answering my text," or something.
This is part of the problem, and I think this is the main part of the problem, by the way, is anxiety. We simply build up this anxiety over, and over, and over again, and the chemicals build up. Then our job is to do whatever we're anxious about so that the chemicals get reabsorbed.
For most people, cortisol is a pretty well-known chemical in our body and our brain. And we know that cortisol is the fight or flight chemical, but it's also in little amounts, not fight or flight at all. It wakes you up. Cortisol is what wakes you up in the morning. You get a little drip of cortisol. During the day, you get cortisol, and it kind of keeps your level of intensity at a pretty good state.
Another interesting study, not by our lab, but another interesting one is that somebody took... They recruited families with a mother, a father, and a teenager. Then what they did is beforehand, they had them fill out all sorts of questionnaires. How many times a day do you check your social media? How much time do you spend on social media? How much time do you spend on email and all sorts of various questions?
They went to sleep. As soon as they woke up, they took a Q-tip, took a swab, saliva swab, put it in a jar, sealed it, put it in the refrigerator, and then eventually sent it into a lab that records how much cortisol, right? They did it right when they woke up, and they did it 30 minutes later. Then they did it other times during the day, but that's not the point.
The interesting point is they were looking at what would cause your cortisol to jump from when you wake up to 30 minutes later. Now, nothing with moms, nothing. No use in general. No use of technology specifically predicted an increase. The dads' email did. Those dads that used more emails showed a bigger response in 30 minutes, which makes sense because they're working, and they get a lot of emails, and first thing in the morning, they got to check them to make sure what's going on.
For teenagers, the only thing that predicted an increase was those who use more social media. So you can already see this building up. You wake up, and you're already anxious. Even the first 30 minutes, you get more and more anxious. You just get more and more anxious. So the anxiety can be very debilitated, and particularly because, I mean, this is not an unknown fact, you can't have a lot of anxiety in you all the time. I mean, it would make you crazy. I mean, if you're always anxious all the time, they'd probably lock you up someplace because anxiety's reached a big peak.
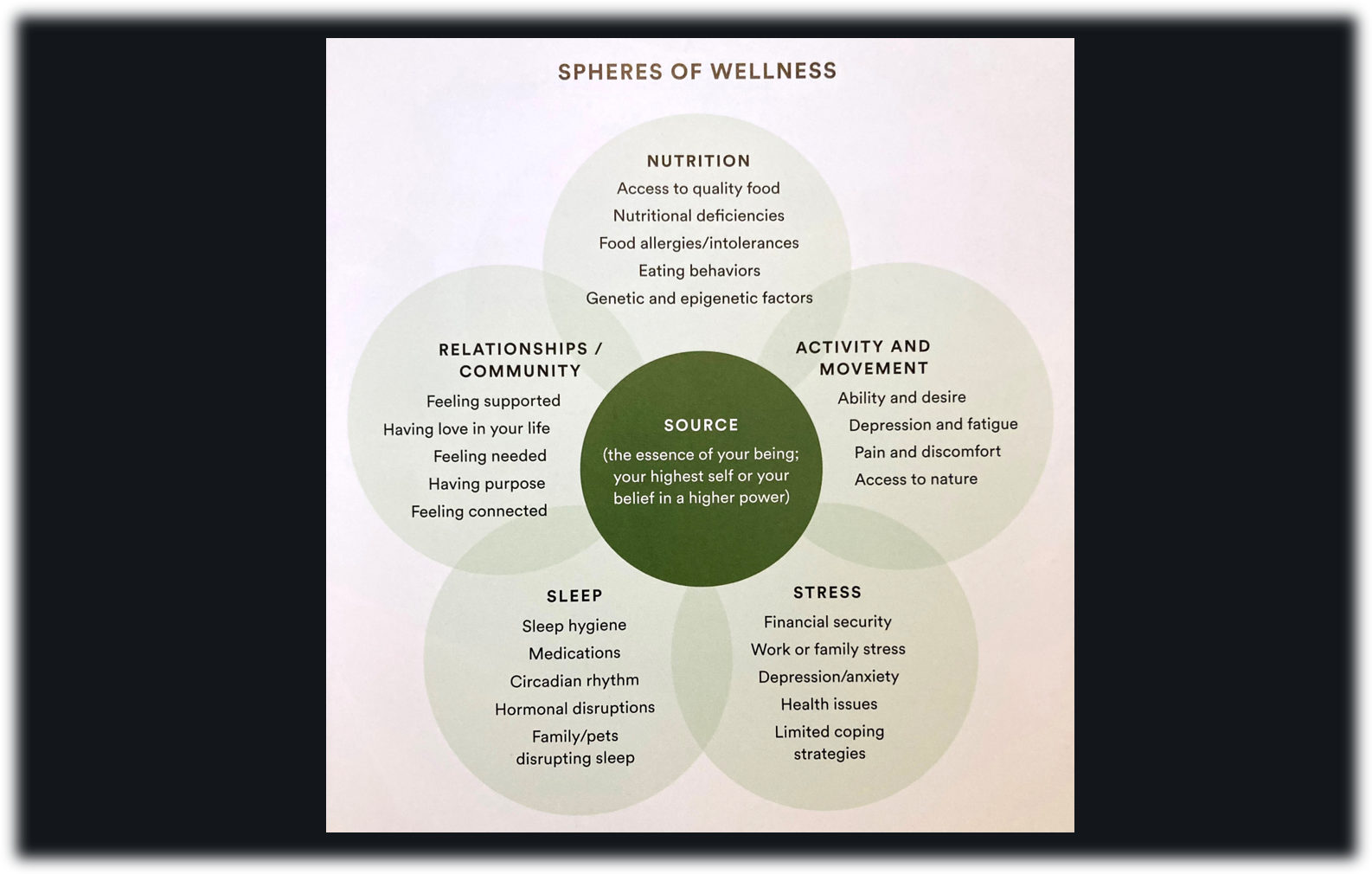
And so, what I have always been interested in is trying to figure out ways to help people be aware of this, first of all, and then figure out a way for them to reduce their anxiety because the anxiety gets in the way of everything. It gets in the way of your thinking, your choice of attention, your multitasking ability, pretty much everything. It all takes place, by the way, right here in the prefrontal cortex, but the anxiety chemicals are buried in the brain and in the body. And in the brain, they're typically right behind here in the amygdala, which then measures your emotions and a bunch of other things.
So, my interest has really moved over the years to trying to figure out what is going on and what can we do to fix it. The first part's easy. The second part's not easy because as I said before, we tried to fix it, tried our hardest. Couldn't do it. We tried. Now, that's not to say that there aren't strategies to do it. I have a lot of strategies that I recommend to people, not a lot, but that we know work. But we're still facing this anxiety reaction all the time.
Jennifer Ghahari: For, I think, a delight for our listeners, we actually are going to hear about two topics from you because it seems that you're kind of budding into a specialist into another field as well. Unfortunately, you were diagnosed with Parkinson's disease a few years ago, and you have started researching this and writing about your own experiences through a blog.
So, I was wondering if you could talk and share with our listeners a little bit about that. What are some of the first signs that you experienced? Especially as a researcher, you're going to have, I think, a different take on this type of diagnosis than someone without your skills.
Larry Rosen: Right. And Parkinson's is a disease. It is a confusing disease because you can exhibit myriad symptoms, and no two people exhibit the same symptoms at all.
Jennifer Ghahari: Oh, wow.
Larry Rosen: I noticed, for example, that when I walked, my left arm did not swing. When we walk, our arms swing back and forth, back and forth. Yeah, they swing. My left arm did not swing, which, I mean, it's a little strange. I also noticed when I was brushing my teeth that my arm was rigid. My left, my other arm was rigid and not moving also.
Jennifer Ghahari: Wow.
Larry Rosen: And didn't really know what it was, but I knew I'd better have an MRI to figure it out. Had an MRI done, and the MRI came up pretty clean in the sense that it really didn't show the Parkinson's because it's hard to do that, but Parkinson's is a biochemical issue. The chemical there, which is interesting, is dopamine.
Now, when we talk about kids being addicted to technology, for example, being addicted, dopamine is the main chemical we talk about. It's also the main chemical that those... part and parcel of Parkinson's. So one of the nice things is they can measure... Technology's so amazing. They can measure with a device sort of like a CAT scan or an MRI, but a simpler one, how much dopamine you have in your brain. They print you a nice, pretty picture, and the pretty picture has this orange-ish stuff showing the active dopamine. It usually looks like two little circles with commas coming out. If you have the requisite amount of dopamine, that's what you'll see. Mine had no commas-
Jennifer Ghahari: Oh, interesting.
Larry Rosen: ... just two circles. So that was pretty interesting. I am a scientist as you can tell from the science t-shirt. I am a scientist. This one says, "Science doesn't care what you believe, by the way," which I think is a good model for people to understand.
I had been looking at dopamine anyway, particularly with video gamers, because it's such an important part of what happens when you're addicted to video games, is this drive for more dopamine, this drive for more dopamine. You got to have it. You got to have it. You got to have it.
Well, so Parkinson's is a dopamine-related problem, and I started thinking about what to do about it. Now, you have to know that I'm a very open person, so I tell everybody everything, and so what I decided to do is to blog about it. I've been writing a blog for Psychology Today for years and years, and not very often, just maybe... Well, they yell at me if I don't do it every 90 days, so try to do it three or four times a year.
I like writing about technology because that's what I do. It's been writing about new generations, and kids, and video games, and all that stuff. All of a sudden, I'm sitting here looking at Parkinson's, and I go, "Well, why don't I write about Parkinson's?" So the first one I wrote called was called something like A Scientist Grapples with Parkinson's Disease because that's what I was grappling with.
I laid out in there some of the symptoms I have. I mean, for example, one's called micrographia. You write very tiny. Your writing gets tinier, and tinier, and tinier. There are other symptomologies that show up. Different people have different ones. Tremors. I have tremors in my left hand, but not my right, which was interesting, but that's not uncommon. Most people just have them on one side or the other to start. Sometimes they migrate.
So, I'm sitting here with a person sitting on my shoulder on this side, being the scientist, looking into it, and the person on this side being the person experiencing it. I thought I'm kind of in a unique place to be able to talk to people about what I'm feeling, and so I wrote that one. I wrote one the second year, and I just posted one for the third year a little late, mostly because I'm doing it kind of for me, my family, my kids, people I know.
I've seen symptoms come and go, more come than go, unfortunately. As you get deeper into Parkinson's and you start reading the research on Parkinson's, there are no two people who have the same Parkinson's. It just isn't. It isn't. Once it's diagnosed, you've can look at things. My neurologist has me always walk down the hall, watches my arm, whether it swings or not, but also watches how I turn to come back. Parkinson's people turn like this in little steps to turn around. I turn... I literally swivel like a ballet dancer. These are some common symptoms that you can see.
One of the interesting things is Parkinson's is a balance issue to people. People who have Parkinson's often fall, and that's really one of the major problems with... And people, by the way, do not die of Parkinson's. They die of something else that Parkinson's brought on, often Alzheimer's, often some form of dementia, often some other neurological problem, fall, hurt themselves. At the very end, you have trouble swallowing.
I just kept thinking, "What can I do to help myself?" Because part of the reading I found was, well, there's this boxing class, and boxing is good for your balance. I went to this boxing class. I joined a boxing class called Rock Steady Boxing. It's made for Parkinson's patients.
Jennifer Ghahari: Wow.
Larry Rosen: It's a franchise. People open their own little gyms or use other gyms. Couple times a week, I was going to this boxing class. It was great fun, by the way, hitting a bag, bam. Just a picture of somebody you don't like, bam.
What happened out of that is... First, the pandemic started, and so you can't be in a closed gym with a bunch of people, but there were a group of us. At that point, there was a group of four of us who'd kind of gotten to know each other, just chatting here and there. We decided to form our own little support group. Now, this is the pandemic, so every week, we met on Zoom. For a year-plus, we met on Zoom.
Then we decided to branch out and meet out in the open where we had lots of fresh air coming and everything. That was an important step, I think, because what that said to me is support is really important. Now, obviously, I get support from my family. I get support from my wife, soon to be my wife. We've been together for 18 years. We're finally getting married.
Jennifer Ghahari: Oh, congratulations.
Larry Rosen: Don't ask me why because I have no idea why we decided to do it, but 18 years seems fine. So they lend support, but it's a different kind of support when you get it from somebody who's experiencing the same thing. We talk about medications. We're all on different medications. We all have different symptomologies. One of the people walked in like this all the time. Why? Because he wasn't taking these meds.
Other people would talk about varying their meds. Their neurologist would let them take maybe a pill in the morning and another half if they felt uncomfortable. The medication, by the way, is exactly the same medication they've been using forever. It's called levodopa, which they always talked about that with Muhammad Ali and various other people who had Parkinson's. Levodopa is the drug of choice. It's actually called Sinemet because it's combined with another drug so you don't get nauseous and constipated, I think, are the two bad things for that.
I started on a very low dose, and my hands shook like this. Also, interestingly enough, my thumb would often stick to my finger, and I would have to pry it off. I've never met anybody with that symptom, by the way. It'd just stick.
Jennifer Ghahari: Oh, wow.
Larry Rosen: I go, "That's weird." Well, I pry it off, and then it's fine.
I have had to increase my Sinemet, my medication quite a bit. The maximum you're supposed to take is 2,000 milligrams. I take 900. My doctor swears that's fine. I'm in a great range. Don't worry about it. We're really good. That took away all my tremors. I rarely have tremors, unless I get stressed. If I get stressed, the tremors come right back.
Jennifer Ghahari: Oh.
Larry Rosen: Yeah. Because stress-
Jennifer Ghahari: Even with medication?
Larry Rosen: Yeah. Stress exacerbates the symptomology that we ha, particularly the tremors. Stress just knocks the tremors back in. Along the way, I mean, I've experienced it. I've written what I've experienced. There's cognitive deficits that I have. There's physical deficits that I have.
The interesting thing is the cognitive deficits are hard to deal with now because I'm 72. How many of the cognitive things that happen to me, like not being able to remember names, happen because I'm 72, not because I have Parkinson's? So, trying to disentangle those is very difficult. You just have to kind of accept that they're either/or and talk to your neurologist about what they may be.
Then over time, I mean, the symptoms come and go. I have some interesting new ones. One's called REM behavioral disorder, which is when your REM sleep, we have movements. When we sleep, Parkinson's patients, those who have this disorder, will act out their dreams. I will pound things. My wife told me last night that she woke me up because she said I was just pounding and talking.
Jennifer Ghahari: Oh, wow.
Larry Rosen: I was just literally acting it out. That's all again caused by the dopamine.
Jennifer Ghahari: Wow. So in addition to these physical and cognitive implications, what about comorbid mental health conditions? Are anxiety and depression common or any other...
Larry Rosen: Yeah, all of them. Anxiety and depression are common. In fact, when I was prescribed my first Sinemet, I was also prescribed an antidepressant-
Jennifer Ghahari: Right off the bat?
Larry Rosen: Right. Because my neurologist said, "You're going to be depressed for a while. Sorry." Then as things went on, I also was prescribed an antianxiety because certain things were making me anxious. So you have to balance the mental health aspects, but they're always going to be there. There's just no way you can skate through this and just go, "Ugh, I'm not feeling bad at all." It's depressing.
It's depressing particularly because the way they show Parkinson's is more end-state Parkinson's Michael J. Fox is not the Parkinson's norm. He's trembling all over the place, and his speech is problematic, and his throat closes up a bit. Yeah, he's not the norm. The norm are people who are like me. They have some symptoms. They try to get rid of the symptoms.
Part of what I'm trying to do in my life is give back because I taught for 45 years, a college profession, and I've done research, and I've participated out there, and given speeches, and all sorts of stuff. I felt like I needed to give back what I knew. Part of it came from our little support group.
I live in San Diego County. There's an organization here called Parkinson's Association of San Diego. There's Parkinson's associations everywhere. One of the things they did is open a mentor program, and so I immediately put my name in to be a mentor. I suggested that I'd rather mentor newly diagnosed people. Interestingly enough, I haven't really mentored any newly diagnosed people, but I've mentored a bunch of people who are really like me, kind of older, scared, concerned, everybody with different symptoms.
I talk to this one guy every week or so on the phone now. When I started talking to him, his mouth movements were not very good. He was a very slow speaker because of it. Over time, it's been interesting because he's now developing speech better, and so he and I can have a conversation where I'm not just sitting there waiting for the next word to come out.
Everybody's different. That's what's so interesting. Everybody's different. I feel like coming from a scientific tradition, I was really raised as a statistician, what that allows me to do is to look at the research and decide whether the research is good or maybe only suggestive. That's an important thing, I think, because research is tricky. Over the 40-some-odd years, plus graduate school, that I was doing research, there are tricks of the trade. There are ways to make a study good. There are ways to make a study bad. There's ways to make conclusions that shouldn't be there.
So, I read those things voraciously. People send them to me, and I read them. I don't talk about them on my blog because I don't want to shame anybody. But I do talk about with new people, here's some new things that are coming up, and I do talk in interviews like this about here's some of the things that might expect.
By and large, it is being diagnosed more, which I think is very interesting. Part of the reason why, by the way, it's diagnosed more is because now we have the testing, the DAT scan to really test it, and we have MRIs that are better. We have tests of fives or something the MRI takes, which is really great stuff, the fine brain stuff.
I will keep writing about it, and I will keep letting people know the symptomology that I have. By the way, because of my cognition problems, I did take a whole neuro workup. I just got the report, and I read part of the report. There are some neurological deficiencies, not horrible ones, but there are some neurological deficiencies, which is helpful for me to understand.
Interestingly enough, attention is one of the major ones right now, and I have a lot of trouble attending. I used to be a great multitasker. Don't do it. Can't do it. I used to think quickly. Sometimes my thoughts get a little muddled, and I have to kind of hold them inside until I get them out. I miss things. I see something on TV, for example, and somebody will say, "What did that person say?" Oh, I don't know. I don't know because my attention waned. So I'm able to say all those things, and I hope people who need it will read it.
Jennifer Ghahari: So those issues that you just spoke of, how do you know what the difference is between a symptom of Parkinson's versus just normal aging-
Larry Rosen: That's the million-dollar-
Jennifer Ghahari: Or there's no real way to know, right?
Larry Rosen: Million-dollar question. No, there's no real way to know. The interesting thing is I think it's good that there's no real way to know because as we get older, those aging symptoms will be there as well as the Parkinson's. Who cares whether it's aging or not? It's still interacting with your Parkinson's.
If I have trouble attending things, it's going to interact with my Parkinson's. If I have trouble remembering names because I can't pull them out of my hippocampus or whatever, it's going to be... Whether it's old age or Parkinson's, it doesn't really matter quite honestly. I mean, most of the people who get Parkinson's are older, so it's all mushed together. How can you tell?
But one of the things I do talk to people about is that they should be very careful to have someone watching over them because part of what happens and because this is dopamine... By the way, we always think of dopamine as the pleasure chemical, but it controls motor motions. And so if you have less dopamine in your body, you have poorer motor motion. One of the first questions the neurologist will ask, "Have you fallen in the last X amount of time?" Because that's a real strong indicator of potential Parkinson's problems.
So, I try to walk more. I try to make sure my balance is there. I also have a spiral staircase in my house, and I'll hold on. At times, I'll take two feet on one step, make sure that I'm not going to fall. I've not fallen yet, but I've definitely stumbled a lot and just been able to grab myself, but I've missed the bottom stair of our stairwell before a couple times. I stumble. Luckily, there's a wall right up there, so I put my hands against the wall. Saved my life.
Those are kind of all things that are individual. The anxiety, by the way, is pretty common. The depression is very common. And so from a psychological point of view, those are the kind of things. Yeah, am I depressed because I'm older? Am I anxious because whatever? Those things are also all tied up in one.
Interestingly enough, because of my work with technology, I'm able to talk about the biochemistry of it because of all the stuff that I've done with the biochemistry of the brain with technology. It's a pretty natural step, I found, to go from looking at that kind of biochemistry to looking at the biochemistry of Parkinson's.
Jennifer Ghahari: Talking about social support and how important that is, you mentioned family, friends. You're part of this boxing group, which morphed into just a social support group. You're also mentoring people. In one of your blogs, you said something like, "I'm not complaining. I'm just reporting." I'm wondering, especially when you're trying to be in a supportive type of setting, whether you're talking to family or in a group, how many people feel like they are actually complaining and they might want to hold back what they're feeling? Is that common or are people more comfortable to talk about things?
Larry Rosen: From my experience with Parkinson's patients, they are embarrassed. In our little group of four... ended up being five. Now, one passed away, so it's four of them.
Jennifer Ghahari: Sorry.
Larry Rosen: We don't meet anymore in the boxing because the person running the boxing program is not vaccinated. I mean, none of us... Even with Parkinson's, you don't want to be anywhere near that stuff that might have an effect on you. There's not been proven a link, but it's still there.
I think that the support you get is the way that you're able to judge aging versus not aging. In our group, there are people in their 60s, 70s, and one is in his 80s. We all reacted differently. I told everybody because that's me. One person only told her husband. That was it. Hadn't told her whole family that she has it. Another person told selective people. I think it's important to be able to see people in a similar situation as you are. I don't know if you know this, but Alan Alda has Parkinson's.
Jennifer Ghahari: Oh, I didn't know.
Larry Rosen: It's funny. He's actually done a lot, and I like what he's been working on. He was in a movie. The movie was the one where Scarlett Johansson and Adam Driver were getting divorced. He was playing Adam's attorney, and so they're sitting at a round table, and you see his right arm is down to the side, and his left arm is here. Then every once in a while, he brings his right arm up, and it's shaking a little, so he put it down. It's a little bit more... That wasn't maybe part of the script, and so they made it as innocuous as possible, but if you go on his Twitter, he talks about it a lot.
Having people do that helps normalize it. I think that's going to be real important for people. I mean, Parkinson's sounds like a really crazy, bad disease, which, I mean, on the whole, it is, but it's not as scary as we always thought it was. We're not going to be Michael J. Foxes. I mean, because he literally has a bad case of the tremors on both sides, as well as speech problems, and all sorts of things. He's at the end, and some of the people I know are spread out in there. I would consider myself maybe not at the other end, but sort of third of the way in because I don't tremor much.
Jennifer Ghahari: And you were diagnosed how long ago?
Larry Rosen: August 2019.
Jennifer Ghahari: Okay. So you have had the disease for a few years now.
Larry Rosen: Okay. So what's interesting is, yes, most people have Parkinson's for a lot longer than they know. One of the first symptoms is loss of sense of smell, and not everybody again, but it's a pretty common symptom. I lost my sense of smell, most of it, 10 years ago, which they would say is because you have Parkinson's.
Jennifer Ghahari: Wow.
Larry Rosen: I don't know how long my left arm wasn't moving because I wasn't paying attention to it. My guess is it was a long time before I was diagnosed. The only reason I was diagnosed is because I felt like there were some things that were just different that I didn't understand neurologically.
Jennifer Ghahari: Wow. That's great. And I appreciate that you're coming on here, and speaking with us, and showing, as you're saying, a more normalized version of Parkinson's, that not everybody's going to have the absolute extreme version, especially right off the bat. So, if anything, this is going to be a really huge help, I think.
Larry Rosen: Michael J. Fox has had it for like 30 years and-
Jennifer Ghahari: Right. Yeah, it's been a long time.
Larry Rosen: Yeah. What I think in the long run is the diagnosis is going to be made more often. By the way, there's all sorts of sub-varieties of Parkinson's, essential tremors. There's a Lewy bodies part. There's a whole bunch of little subcategories. We can have those or full-out Parkinson's. They have different symptoms and different effects.
I think because of our technology now, and because we're just more aware of it... I mean, Michael J. Fox is out there. Other people are out there talking about Parkinson's. Because of that awareness, I think more people then go to the doctor and will be diagnosed. We'll get better ways of diagnosing them, and we'll get better ways of treating them.
There are a tremendous number of research studies going on right now on other treatments other than drug treatments. For example, there's something called DBS, direct brain stimulation, where you literally have a little thing here, and it stimulates... It's like a nine-volt battery and stimulates the prefrontal cortex, which has been shown to help with your thinking and your attention abilities if one of the symptoms is you're losing your attention.
I mean, I have high hopes that the more we see out there, the more we'll understand out there, but it's scary. I mean, I would tell anybody that has Parkinson's. The first thing I would say is, "I bet you're scared." The answer is always, "Yeah, I'm scared to death." They have a reason to be. I mean, it's not a death sentence, but in general, people who get Parkinson's, they live maybe 20, 30 years with Parkinson's, or it can go really quickly. You just don't know.
Again, the medications are much better. The medications are better. There's lots of other meds besides the one I'm taking. The one I'm taking just is the base one you start on. If that doesn't work, they can give you other meds on top of it, or interestingly enough, the meds stop working typically after... I think Sinemet, they say, in general, stops working maybe every about five years with that. You have to find something else.
Jennifer Ghahari: Yeah. I think, as you said, it's almost the fear of the unknown. That's the biggest drive of anxiety for people, and so I think things like this where you're helping disseminate information and just experiences is a really huge help for people.
Larry Rosen: And one of the things that I would recommend is... The Parkinson's Association of San Diego has done a really nice service for people, and what they've done is they've had professionals record very short videos, we know our attention span is way too short these days, eight, 10-min videos on different symptoms and different kind of things that happen. It's just pasd.org, I think. They're free. You can go look at the videos. There's probably 30 or 40 of them, maybe even more.
Jennifer Ghahari: Wow.
Larry Rosen: The PA for my doctor does a few, and other people who know what they're doing do a few. Then my doctor, my neurologist is involved in lots of research too along with it. So I get to kind of eavesdrop and hear what she's finding. She talks on there about her research. People talk about the REM behavioral disorder and what it means. People talk about how to know when your medication's not working. So they're just little blurbs. I encourage people... I think it's a really great idea to just go there and harvest what we can.
Now, having said that, when I was diagnosed, I did no reading. In retrospect, I was scared to death and I didn't want to know. Everybody else read for me. My kids reported. My wife reported. Everybody read for me. Then at some point after about six months, I found that I was able to dive in and see what's there. Also, I mean, I encourage people to not be afraid to say, "I'm afraid."
Jennifer Ghahari: Wow. Thank you. So psychologist, who's an expert in technology, someone who's battling Parkinson's, do you have any parting words of advice or anything else that you'd like to share with our listeners?
Larry Rosen: Well, on both sides, I can share a lot about the technologist stuff, but I think keep track of what you're feeling. If you need to, take a diary. Keep track of it in a diary. Mark down when something odd happens, something weird happens. It may be Parkinson's. It may be not. At least, it's noted.
Don't spend a lot of time reading research because it's in its infancy. We're talking about really the last 10 years maybe that there's been this new emphasis on Parkinson's, even though Michael J. Fox had his foundation for quite a while, but it's pretty much a new phenomenon. When you say to somebody, "Oh, I have Parkinson's," say, "Oh, my uncle had Parkinson's, and my mother's sister had Parkinson's." Everybody knows somebody that had Parkinson's.
And to just realize it's not a death sentence, but you also need to kind of be aware of your body and your mind because you can just go on gleefully unaware, and then the symptoms will definitely get worse left untreated. What you want to do is try to get the best treatment possible and really trust that...
You're not doing this through your family doctor or your internist. You're doing this through a neurologist who knows Parkinson's, whether it takes... Even if you have some of these symptoms, and you try to get an appointment and you can't get an appointment for four months, don't worry about it. Nothing's going to much change in four months maybe.
Keep track of your symptoms. Keep track of everything. Don't study the research on it. Go look at how you can diagnose Parkinson's. There's lots of things that talk about how you walk or do this. (Moves his hands) My right is faster than my left.
Jennifer Ghahari: Oh.
Larry Rosen: Typing, my right is better than my left. I can't type anymore. I mean, I can type. It's just I make lots of mistakes. Keep track of your symptoms. Keep track of them, and write them down. Make sure that you are being as dispassionate as you can, but yet accept the support of other people. Don't ever let somebody tell you you're going to die of Parkinson's because they will. They'll say, "Oh, my uncle had it for 20 years and then died."
Jennifer Ghahari: Right. Well, thank you so much. If anybody wants to read more about Dr. Rosen's research or read more about his blog, you can do so at www.drlarryrosen.com, and we'll have that link on our site.
Larry Rosen: And the doctor is just D-R. Mention that maybe.
Jennifer Ghahari: Oh, perfect. Thank you. Yeah.
Larry Rosen: Please feel free to message me too. I mean, I enjoy talking to people about this because I think I can maybe not... Don't I'm a great helper, but I'm a pretty good listener.
Jennifer Ghahari: Aw.
Larry Rosen: And I think that's important.
Jennifer Ghahari: It does make all the difference, definitely.
Larry Rosen: Yeah.
Jennifer Ghahari: Thank you so much, Dr. Rosen, and we wish you all the best.
Larry Rosen: Thanks. Thanks for having me on.
Jennifer Ghahari: Thank you.
Please note: The views expressed by the interviewee are for educational and informational purposes only, are not meant to diagnose or treat any condition, and do not necessarily reflect the views of Seattle Anxiety Specialists, PLLC.
Editor: Jennifer (Ghahari) Smith, Ph.D.