Major Depressive Disorder (MDD)
Overview
One of the most common psychological issues, major depressive disorder (MDD) (i.e., depression, major depression or clinical depression) affects more than 300 million persons globally.[1] This mood disorder causes severe symptoms that affect how one feels, thinks, and handles every day activities, such as sleeping, eating, or working.[2] Depression leads to a variety of emotional and physical problems that decrease one’s ability to function at work and at home as well as a loss of interest in activities that were once enjoyed.[3] One may contemplate if life is not worth living.[4]
The most prominent symptoms of depression are a severe and persistent low mood, profound sadness, or a sense of despair. While one’s mood may appear as irritability, major depression is more than just a passing "bad day" or temporary sadness.[5] Depression is a serious medical illness; not a weakness of character one can simply "snap out of".[6] To be diagnosed with depression, symptoms must be present for at least two weeks;[7] however, usually they persist much longer: months or even years. Further, a major depressive episode may occur just once in a person's life or repeatedly return.[8] Fortunately, depression is treatable.[9] Depending on the individual case, battling depression may require long-term treatment, with the majority of persons improving with medication and/or psychotherapy.[10]
Diagnosis
Depression affects one-in-15 adults (6.7%) in any given year, with one-in-six (16.6%) will experiencing depression at some point during their lifetime. While MDD can occur at any time, it tends to first appear during the late teens to mid-20s. Women are more likely than men to experience depression, with studies indicating one-third of women experience a major depressive episode in their lifetime.[11] However, it is important to note that while more women than men are typically diagnosed with depression, this may be due to more women seeking treatment.[12] Further, there is a high degree of heritability (approximately 40%) when one’s first-degree relatives have depression.[13]
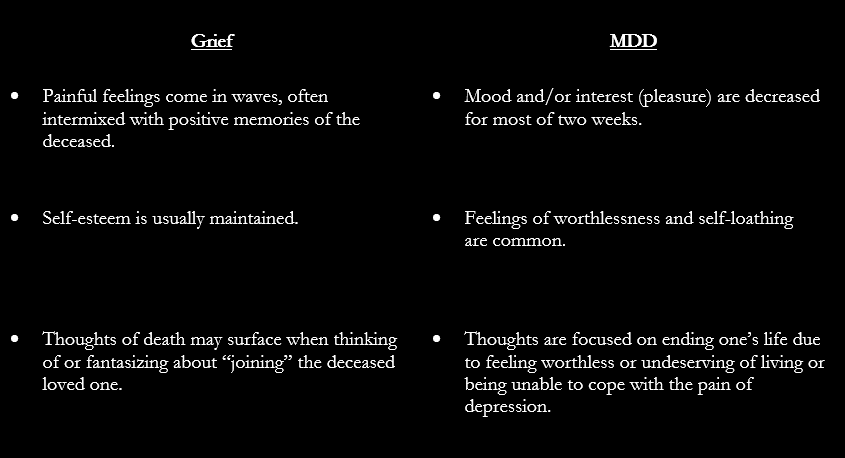
The distinction between MDD and sadness or grief/bereavement should be noted. While the death of a loved one, loss of a job or the cessation of a relationship may be difficult to endure, feelings of sadness or grief are normal psychological responses in such situations. Those experiencing loss tend to describe themselves as being “depressed,” however this is not the same as a clinical diagnosis of MDD. Although the manifestations of grief resemble that of major depression, they also differ in key ways:[14]
While differences do exist between the two conditions, grief and depression can co-exist. The death of a loved one, loss of a job or victimization in a physical assault or major disaster can lead to MDD. Further, when grief and depression co-occur, the severity and duration of grief is more significant than grief without depression. Distinguishing between grief and depression is essential to helping receive the help, support or treatment one needs.[15]
Differing from MDD, the National Institutes of Health (NIH) notes following forms of depression may develop under unique circumstances, such as:[16]
Persistent depressive disorder (also called dysthymia) is a depressed mood that lasts for at least two years. A person diagnosed with persistent depressive disorder may have episodes of major depression along with periods of less severe symptoms, but symptoms must last for two years to be considered persistent depressive disorder.
Postpartum depression is a serious condition. While many women experience relatively mild depressive and anxiety symptoms following birth, these typically clear within two weeks post-delivery. Women with postpartum depression experience major depression during pregnancy and/or after delivery. The feelings of extreme sadness, anxiety, and exhaustion that accompany postpartum depression may make it difficult for new mothers to complete daily care activities for themselves and/or for their babies.
Psychotic depression occurs when a person has severe depression plus some form of psychosis, such as having disturbing false fixed beliefs (i.e. delusions) or hallucinations. One’s psychotic symptoms typically have a depressive “theme,” such as delusions of guilt, poverty, or illness.
Seasonal affective disorder (SAD) is characterized by the onset of depression during the winter months, when one experiences less natural sunlight. This form of depression generally subsides during spring and summer. SAD is typically accompanied by social withdrawal, increased sleep, and weight gain, and tend to predictably returns every year in those with this disorder.
Bipolar disorder differs from depression, but it is included in this list is because those with bipolar disorder experience episodes of extremely low moods that meet the criteria for MDD (called “bipolar depression”). A key difference between these two conditions is that one with bipolar disorder also experiences extreme highs (euphoric or irritable) moods called “mania” or a less severe form called “hypomania.”
A primary care physician or a mental health professional can typically identify MDD by asking questions about medical history and symptoms.[17] A blood test might be done to make sure the depression is not due to a medical condition like a thyroid problem or a vitamin deficiency (reversing the medical cause would alleviate the depression-like symptoms). Complete evaluations explore specific symptoms, medical and family histories as well as cultural and environmental factors with the goal of arriving at a diagnosis and planning a course of action.[18] If depression is not treated, it can become chronic; treatment can both lessen the length and severity of a depressive episode.[19]
Signs and Symptoms
The following clinical symptoms of MDD must present nearly continually, for at least two weeks,[20] and represent a change in your previous level of functioning:[21-24]
Feeling sad or having a depressed mood
Angry outbursts, irritability or frustration, even over small matters
Anxiety, agitation or restlessness
Loss of interest or pleasure in activities once enjoyed
Changes in appetite — weight loss or gain unrelated to dieting
Sleep disturbances, including insomnia or sleeping too much
Loss of energy or increased fatigue
Increase in purposeless physical activity (e.g., inability to sit still, pacing, handwringing) or slowed movements or speech (these actions must be severe enough to be observable by others)
Feelings of hopelessness or pessimism
Feelings of guilt, worthlessness or helplessness
Difficulty thinking, concentrating or making decisions
Aches or pains, headaches, cramps, or digestive problems without a clear physical cause and/or that do not ease even with treatment
Thoughts of death, suicide attempts or plans to commit suicide
Not everyone who is depressed experiences every symptom; some experience only a few symptoms while others experience many.[25] Symptoms tend to be severe enough to cause noticeable complications in one’s day-to-day activities (e.g., work, school, social activities or personal relationships.)[26] Several persistent symptoms, in addition to low mood, are required for a diagnosis of MDD; but people with only a few, but distressing, symptoms may benefit from treatment of their subsyndromal depression. The severity and frequency of symptoms and how long they last will vary depending on the individual and their particular illness. Symptoms also vary dependent on the stage of one’s illness.[27]
Depression Symptoms in Children and Teens
Common signs and symptoms of depression in children and teenagers are similar to those of adults, although differences do exist.[28]
In younger children, symptoms of depression may include: sadness, irritability, clinginess, worry, aches and pains, refusing to go to school, and/or being underweight.
In teens, symptoms may include: sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, the use of recreational drugs and/or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression Symptoms in Older Adults
Depression is not a normal occurrence of aging nor should it be down-played or ignored. Due to typical social norms and conventions, MDD is often undiagnosed and untreated in older adults, particularly as one may feel ashamed and reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:[29]
Memory difficulties or personality changes
Physical aches or pain
Fatigue, loss of appetite, sleep problems or loss of interest in sex — not caused by a medical condition or medication
Often wanting to stay at home, rather than going out to socialize or doing new things
Suicidal thinking or feelings, especially in older men
Causes
Although major depressive disorder is prevalent worldwide, little is known about its etiology.
Ranjbar et al. (2013) noted that, “levels of certain trace elements are associated with the pathogenesis of some diseases,” and specifically their case–control study of 60 male patients with MDD and control subjects found significant differences in their bloodwork. Those with MDD had significantly higher levels (p < 0.001) of Cu, Cr, and Al compared with the Control group. Further, there were significantly lower levels (p < 0.001) of Zn, Ni, Mn, Mg, vitamin E, and vitamin A in MDD patients. In addition, high Cu/Zn ratio (p < 0.05) was observed with the depressive disorder patients. Summarizing their findings, they suggest “Cu and Zn seemed to have a crucial role in understanding the pathogenesis of depressive disorders, where Cu/Zn ratio could have an important role in the diagnosis and monitoring of MDD. Moreover, the results suggest that the reduction in the antioxidant vitamin E leads to increased risk of MDD. Finally, more studies on using trace element supplementation would be suggested to clarify their effect, in order to improve the therapy of MDD.”[30]
A stressful life event may trigger an episode of depression, but it often does not appear to present as related to a specific event. Additionally, while there is no way to prevent MDD, early detection is beneficial as treatment can both reduce symptoms and aid in preventing its reoccurrence.[31]
The Mayo Clinic notes that as with many mental disorders, a variety of factors may be involved, such as:[32]
Biological Differences - People with depression appear to have physical changes in their brains. The significance of these changes is still uncertain, but may eventually help pinpoint causes.
Brain Chemistry - Neurotransmitters are naturally occurring brain chemicals that likely play a role in depression. Recent research indicates that changes in the function and effect of these neurotransmitters and how they interact with neurocircuits involved in maintaining mood stability may play a significant role in depression and its treatment.
Hormones - Changes in the body's balance of hormones may be involved in causing or triggering depression. Hormone changes can result with pregnancy and during the weeks or months after delivery (postpartum) and from thyroid problems, menopause or a number of other conditions.
Inherited Traits - Depression is more common in people whose blood relatives also have this condition. Researchers are trying to find genes that may be involved in causing depression.
While there's no absolute way to prevent depression, the following strategies may help:
Take steps to control stress, increasing your resilience while boosting self-esteem.
Reach out to trusted family and friends, especially in times of crisis, to help during difficult times.
Get treatment at the earliest sign of a problem to help prevent depression from worsening.
Consider getting long-term maintenance treatment to help prevent a relapse of symptoms.
Risk Factors
Current research suggests that depression is caused by a combination of genetic, biological, environmental, and psychological factors. Many chronic mood and anxiety disorders in adults begin as high levels of anxiety in children. Depression, especially in midlife or older adults, can co-occur with other serious medical illnesses, such as diabetes, cancer, heart disease, and Parkinson’s disease. These conditions are often worse when depression is present. Further, medications taken for a physical illness may cause side effects, contributing to depression.[33]
Common risk factors that increase the development or triggering of MDD include:[34-36]
Biochemistry: Differences in certain chemicals in the brain may contribute to symptoms of depression.
Genetics: Depression can run in families. For example, if one identical twin has depression, the other has a 70% chance of developing the illness at some point in their life. Blood relatives with a history of depression, bipolar disorder, alcoholism or suicide can also be precursors to developing MDD.
Personality: People with low self-esteem, self-critical, who are easily overwhelmed by stress, or who are generally pessimistic appear to be more likely to experience depression.
Environmental Factors: Continuous exposure to violence, neglect, abuse or poverty may make some people more vulnerable to depression. The death or loss of a loved one, a difficult relationship, or financial problems can also contribute to MDD. Certain chronic illnesses, medications as well as abuse of alcohol or recreational drugs may also contribute to the manifestation of depression.
Complications
MDD is a serious disorder that tends to exacerbate if untreated, resulting in emotional, behavioral and health problems. Examples of complications associated with depression include:[37,38]
Excess weight or obesity, which can lead to heart disease and diabetes
Pain or physical illness
Alcohol and/or drug misuse
Anxiety, panic disorder or social phobia
Family conflicts, relationship difficulties, and work or school problems
Difficulty of mood regulation
Sexual dysfunction
Social isolation
Suicidal feelings, suicide attempts or suicide
Self-mutilation, such as cutting
Premature death from medical conditions
Treatment and Therapeutic Options
Depression, even the most severe cases, can be treated.[39] Between 80% and 90% percent of people with depression eventually respond well to treatment with nearly all patients attaining some relief from their symptoms.[40] Earlier treatment for MDD correlates with greater efficacy. Major depression is usually treated with medications, psychotherapy, with a combination of the two producing the most effective treatments in many cases. If these treatments do not reduce one’s symptoms, electroconvulsive therapy (ECT) and other brain stimulation therapies may be undertaken.[41]
Medications
A person’s brain chemistry may contribute to their depression. Antidepressants can modify one’s brain chemistry to correct symptoms of MDD. These medications are not sedatives, “uppers” or tranquilizers, nor are they habit-forming.[42]
Selective serotonin reuptake inhibitors (SSRIs) are commonly the first line of pharmaceuticals used to treat MDD. SSRIs include: fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa) and escitalopram (Lexapro). Compared with previous generations of antidepressants, these have been found to be relatively easy to take. However, SSRIs are known to cause problems with sexual functioning, nausea, as well as an increase in anxiety in the early stages of treatment.
Other effective antidepressants include bupropion (Wellbutrin), venlafaxine (Effexor), mirtazapine (Remeron) and duloxetine (Cymbalta). Additionally, older classes of antidepressants, such as tricyclic antidepressants and monoamine oxidase inhibitors, are still in use. These medications are as effective as the newer ones and can be very useful when someone has not responded well to other treatments.
Determining the proper medication can take time. It usually takes at least two to six weeks of taking an antidepressant to see improvement and it may take several trials to find the medication that works best for an individual. A combination of two different medications may be used in conjunction: two antidepressants; or an antidepressant along with a mood stabilizer, such as lithium (sold under several brand names) or valproic acid (Depakene, Depakote). Further, if psychotic symptoms are present, a doctor may prescribe an antipsychotic medication such as: haloperidol (Haldol), risperidone (Risperdal), ziprasidone (Geodon), aripiprazole (Abilify) and olanzapine (Zyprexa). Additionally, once the right medication has been determined, it may take a few months to find the proper dose and achieve greatest benefit from it.[43] Psychiatrists typically recommend medication be continued for a minimum of six months after symptoms of MDD have improved. Longer-term maintenance treatment may be suggested to decrease one’s risk of future episodes, particularly for those at high risk.[44]
Antidepressant cessation should never be attempted without the guidance of a doctor. Stopping antidepressants without the supervision of one’s doctor can lead to a relapse in. Antidepressant dosage must be properly tapered to ensure safe withdrawal and with minimal side effects.
Those suffering from MDD should not engage in taking dietary supplements, especially while taking an antidepressant, unless first discussing it with their physician. Although the herb St. John’s Wort it is a top-selling botanical product, the FDA has not approved its use as an over-the-counter or prescription medicine for depression; there are serious concerns about its safety and effectiveness. Other natural products sold as dietary supplements, including omega-3 fatty acids and S-adenosylmethionine (SAMe), remain under study but have not yet been proven safe and effective for routine use.[45]
Antidepressants and Suicide Risk
In some cases, children, teenagers, and young adults under 25 may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. This warning from the U.S. Food and Drug Administration (FDA) also says that patients of all ages taking antidepressants should be watched closely, especially during the first few weeks of treatment.[46]
Paradoxically, not utilizing an antidepressant due to increased risk of suicide can also lead to an increased risk of suicide if one’s MDD is left improperly treated. Independent of this debate, it is important to monitor treatment closely, immediately reporting any troubling symptoms or worsening mood to one’s doctor.[47]
Psychotherapies
Several types of psychotherapy (i.e., talk-therapy or counselling) can help those with MDD. Examples of evidence-based approaches specific to the treatment of depression include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and problem-solving therapy.[48]
For moderate to severe depression, psychotherapy is often used in conjunction with antidepressant medications. Psychotherapy may involve only the individual with MDD but can include others such as in the case of family- or couples-therapy. Group therapy has been found to be beneficial by bringing people with similar illnesses together in a supportive environment, and by learning how others cope in similar situations.[49]
Depending on the severity of the depression, treatment length ranges from a few weeks to much longer. Typically, significant improvement can be achieved in 10 to 15 sessions.[50]
Brain Stimulation Therapies
If medications do not reduce the symptoms of MDD, electroconvulsive therapy (ECT) may be an option to explore. According to the NIH:[51]
ECT can provide relief for people with severe depression who have not been able to feel better with other treatments.
In some severe cases where a rapid response is necessary or medications cannot be used safely, ECT can even be a first-line intervention.
Once strictly an inpatient-procedure, ECT is now often performed on an outpatient basis. This treatment consists of a series of sessions, typically three times a week, for a duration of two to four weeks.
ECT may cause some side effects, including confusion, disorientation, and memory loss. Usually these side effects are short-term, but sometimes memory problems can linger, for a few months following a course of treatment.
ECT is not painful, and one cannot feel the electrical impulses. Before ECT begins, a patient is put under brief anesthesia as well as given a muscle relaxant. Within one hour after the treatment session (which takes a few minutes) one is awake and alert.
Advances in ECT devices and methods have made modern ECT safe and effective for the vast majority of patients. It is important to discuss and understand the potential benefits and risks before giving informed consent ECT treatment.
The practice of ETC has been used since the 1940s. Research has led to major improvements in this therapy, with recognition of its effectiveness as mainstream treatment and not something to be sought as a “last resort.”[52]
Other, more-recently introduced types of brain stimulation therapies used to treat medicine-resistant depression include repetitive transcranial magnetic stimulation (rTMS) and vagus nerve stimulation (VNS).[53]
Self-Help and Coping Strategies
To further reduce one’s symptoms of MDD, the NIH recommends some actions that may help during the treatment of depression, including:[54]
Exercising and being active.
Setting realistic goals for oneself.
Spending time with others and confiding in a trusted friend or relative.
Trying not to isolate oneself and let others help.
Expecting one’s mood to improve gradually, not immediately.
Postponing important decisions, such as getting married or divorced, or changing jobs until symptoms of MDD have subsided. Discussing decisions with others who know you well and have a more objective view of your situation can be helpful.
The American Psychiatric Association adds the following recommendations to reduce symptoms of MDD:[55]
Obtaining regular sleep patterns and enough quality hours of sleep per night.
Avoiding alcohol, which is a depressant.
With proper diagnosis and treatment, the vast majority of people with major depressive disorder will overcome it. If one is experiencing symptoms of depression, they should reach out to their family physician or psychiatrist as soon as possible to request a thorough evaluation.
Contributed by: Jennifer (Ghahari) Smith, Ph.D.
References
1 World Health Organization, Mental disorders (2018) Archived from the original on 18 May 2015.
2 “Depression,” National Institute of Mental Health. (accessed 11-15-20). www.nimh.nih.gov/health/topics/depression/index.shtml
3 “What is Depression,” American Psychiatric Association. (accessed 11-17-20). www.psychiatry.org/patients-families/depression/what-is-depression
4 “Depression (Major Depressive Disorder),” Mayo Clinic. (accessed 11-17-2020). www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
5 “Major Depression,” Harvard Health Publishing. (accessed 11-16-2020). www.health.harvard.edu/a_to_z/major-depression-a-to-z
6 “Depression (Major Depressive Disorder),” Mayo Clinic.
7 “Depression,” National Institute of Mental Health.
8 “Major Depression,” Harvard Health Publishing.
9 “What is Depression,” American Psychiatric Association.
10 “Depression (Major Depressive Disorder),” Mayo Clinic.
11 “What is Depression,” American Psychiatric Association.
12 “Depression (Major Depressive Disorder),” Mayo Clinic.
13 “What is Depression,” American Psychiatric Association.
14 Ibid.
15 Ibid.
16 “Depression,” National Institute of Mental Health.
17 “Major Depression,” Harvard Health Publishing.
18 “What is Depression,” American Psychiatric Association.
19 “Major Depression,” Harvard Health Publishing.
20 “Depression,” National Institute of Mental Health.
21 Ibid.
22 “Major Depression,” Harvard Health Publishing.
23 “What is Depression,” American Psychiatric Association.
24 “Depression (Major Depressive Disorder),” Mayo Clinic.
25 “Depression,” National Institute of Mental Health.
26 “Depression (Major Depressive Disorder),” Mayo Clinic.
27 “Depression,” National Institute of Mental Health.
28 “Depression (Major Depressive Disorder),” Mayo Clinic.
29 Ibid.
30 Ranjbar E, Kasaei MS, Mohammad-Shirazi M, Nasrollahzadeh J, Rashidkhani B, Shams J, Mostafavi S, Mohammadi MR (2013) Effects of zinc supplementation in patients with major depression: a randomized clinical trial. Iran J Psychiatry 8(2):73–79
31 “Major Depression,” Harvard Health Publishing.
32 “Depression (Major Depressive Disorder),” Mayo Clinic.
33 “Depression,” National Institute of Mental Health.
34 Ibid.
35 “Depression (Major Depressive Disorder),” Mayo Clinic.
36 “What is Depression,” American Psychiatric Association.
37 “Depression (Major Depressive Disorder),” Mayo Clinic.
38 “Major Depression,” Harvard Health Publishing.
39 “Depression,” National Institute of Mental Health.
40 “What is Depression,” American Psychiatric Association.
41 “Depression,” National Institute of Mental Health.
42 “What is Depression,” American Psychiatric Association.
43 “Major Depression,” Harvard Health Publishing.
44 “What is Depression,” American Psychiatric Association.
45 “Depression,” National Institute of Mental Health.
46 “Depression,” National Institute of Mental Health.
47 “Major Depression,” Harvard Health Publishing.
48 “Depression,” National Institute of Mental Health.
49 “What is Depression,” American Psychiatric Association.
50 Ibid.
51 “Depression,” National Institute of Mental Health.
52 “What is Depression,” American Psychiatric Association.
53 “Depression,” National Institute of Mental Health.
54 Ibid.
55 “What is Depression,” American Psychiatric Association.