Impact of COVID-19 on Stress in the Seattle Community
Jennifer M. Ghahari, Ph.D. and Blake Thompson, LMHC
Seattle Anxiety Specialists, PLLC
This article is a summary of the survey research we’ve conducted on the impacts of the COVID-19 pandemic on the stress of the Seattle Community. Based on responses from well over a thousand adults in the area, it focuses on certain psychological impacts of the pandemic and will be of particular relevance to Psychologists, Psychiatrists, and others working in Mental Health as they work to respond to the growing therapy and counseling needs of the community.
The article is optimized for mobile. If you’re reading on a P.C., you can click here to download a pdf version.
INTRODUCTION
The Novel Coronavirus pandemic has led to unprecedented dismay regarding physical and mental health as well as economic crises. Washington state, the first in the country to become impacted by COVID-19, has been most-greatly impacted in Seattle, King County. Seattle Anxiety Specialists, PLLC, (SAS) has developed and conducted exploratory empirical research to examine the psychological consequences of the pandemic on residents of Seattle and surrounding areas. By understanding how residents have been most-impacted by the Coronavirus pandemic, therapists and researchers at SAS will seek to develop and offer community-wide support programs, mental health resources and further efforts to lessen and ease psychological trauma caused by the COVID-19 virus.
BACKGROUND: COVID-19 IN WASHINGTON STATE
On January 21, 2020 the Centers for Disease Control and Prevention (CDC) and the Washington State Department of Health announced the first case of COVID-19 in Washington state.1 Due to the ease of transmission of the virus and risk of severe complications (including death), Washington Governor Jay Inslee issued a “Stay Home, Stay Healthy” order on March 23rd in an attempt to stop the spread of the virus.2 Within a mere three months of COVID-19 appearing in Washington, as of April 20th, all 50 states have reported cases of the virus to the CDC.3
“Coronavirus disease 19” (also called SARS-CoV-2, and abbreviated “COVID-19”) is a pandemic respiratory disease that is currently spreading from person-to-person across the globe. Coronaviruses are a large family of viruses that are common in people and different species of mammals (including: camels, cattle, cats and bats.) Rarely, animal coronaviruses can infect people and then spread between people (such as with MERS-CoV, SARS-CoV and now SARS-CoV-2).4 Due to there being little to no pre-existing immunity against COVID-19 worldwide, this pandemic has spread quickly and sustainably across the globe. Thus, on March 11, the COVID-19 outbreak was characterized by the World Health Organization (WHO) as a pandemic.5
Pandemics begin with an investigation phase, followed by recognition, initiation and acceleration phases. The peak occurs at the end of the acceleration phase, followed by the deceleration phase (in which there is a decrease in cases.)6 While it’s expected that the COVID-19 epidemic may hit its peak in in Washington state during May, increases would continue should the “stay at home orders” cease too quickly. Initial modeling suggested a possible high that forecasted more than 1,600 deaths at the peak of the virus in the state. At the beginning of April, new models calculated by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington's School of Medicine, suggested the state could reach the total projected COVID-19 deaths as early as mid-May and the number of projected deaths would drop significantly in Washington - but added that assessment would be contingent on extended social distancing in the state. Dr. Chris Murray, Director for IHME said the new data shows that social distancing and stay at home orders have been working to reduce the spread of COVID-19 in Washington, particularly in King and Snohomish Counties.7 Projections have been last updated by IHME as of May 12th, estimating Washington’s total deaths as of August 4th could be as high as nearly 1,200 persons. 8
As of April 18th, at the time SAS’ survey was conducted, Washington state’s Department of Health reported a total of 11,790 cases of coronavirus, with 634 confirmed deaths from the virus in the state. The majority of cases (5,135 or nearly 44%) and deaths (346 or nearly 55%) have occurred in King County, where the populous Seattle is located. Following King County, those hit with the highest confirmed cases and deaths include: Snohomish (2,101 / 94) and Pierce (1,109 / 32).9 Those at the highest risk for severe illness from COVID-19 include: people 65 years and older; those living in a nursing home or long-term care facility and those of all ages with serious underlying medical conditions.10
Reported by Washington state’s Department of Health, patients aged 60 and older were most-likely to succumb to COVID-19. While only 35% of confirmed cases were in those aged 60 and older, this cohort comprised 92% of the state’s deaths. Those under the age of 40 appear to be less affected by COVID-19’s morbidity.11
BACKGROUND: PSYCHOLOGICAL IMPACTS OF THE COVID-19 PANDEMIC
During the COVID-19 outbreak, stress and anxiety levels have increased across the community and particularly for those at higher risk for severe illness and with underlying health conditions. Older adults as well as those with disabilities are at increased risk for having mental health concerns, such as depression. Taking a physical toll, mental health issues often manifest and present themselves as physical ailments, such as headaches, stomachaches and/or cognitive problems (such as difficulty concentrating.) Moreover, doctors are more-likely to miss mental health concerns among those in the increased-risk category as their disability and age tend to be viewed as the primary contributor to presented physical ailments. Namely, depression can be mistaken as a normal part of aging in older adults.12
Aside from overall stress and anxiety, common psychological reactions to COVID-19 have formed due to a myriad of causes. Firstly, there is a concern about protecting oneself as well as family and friends. Further, patients often have a sense of guilt if loved ones assist them with activities of daily living. Disruptions in regular medical care or community services impact those who were already medically challenged in some regard, dependent on frequent appointments and assistance. Moreover, feeling socially isolated takes on a psychological toll particularly for those who live alone or are in need of assistance and who are now facing less interactions due to community-wide stay-at-home orders. Further, those facing increased levels of distress are often those who: have had pre-existing mental health concerns (which began prior to the outbreak); live in lower-income households; have language barriers; and experience stigma because of age, race, ethnicity, disability or perceived likelihood of spreading COVID-19.13
Those coming out of quarantine also tend to face severe stressors, regardless if they may have been exposed to COVID-19 and have not gotten sick. Emotional reactions to coming out of quarantine may include: having mixed emotions, including relief; stress from the experience of being monitored for signs and symptoms of COVID-19; sadness, anger, and/or frustration because friends of those close to you have fears of contracting the disease from contact with you, although you have been determined not to be contagious; and guilt about not being able to perform normal work or parenting duties during quarantine.14 Forced isolation, coupled with the fear of possibly having the Coronavirus, is particularly daunting and can be a significant stressor and manifest with both mental and physical ailments. As such, the CDC has cited common signs of distress during this time, including:
Feelings of numbness, disbelief, anxiety or fear.
Changes in appetite, energy, and activity levels.
Difficulty concentrating.
Difficulty sleeping or nightmares and upsetting thoughts and images.
Physical reactions, such as headaches, body pains, stomach problems, and skin rashes.
Worsening of chronic health problems.
Anger or short-temper.
Increased use of alcohol, tobacco, or other drugs.15
BACKGROUND: FINANCIAL INSECURITY AND UNEMPLOYMENT
Approximately 10% of workers have lost their jobs mid-March to mid-April, due to the economic effects of the COVID-19 pandemic.16 With over 10 million people currently seeking jobless benefits17, this is one of the largest and fastest incidence of job losses on record in the United States.18 Washington state has been hit particularly hard by the Coronavirus, with nearly 1 million weekly claims filed, as of April 26th. Washington’s Employment Security Department reported receiving 20,000 calls a day19, utilizing extended resources available such as using evening hours and Sundays to process claims.20
A myriad of workers has been affected by the Coronavirus. According to an analysis conducted by the Institute for Women’s Policy Research, about 60% of job losses were experienced by women.21 The IWPR report added that women lost jobs in four sectors, while employment for men rose, within: educational and health services; financial services; construction; and information. However, men lost more jobs than women in the areas of: wholesale trade, mining and logging. Job losses have also disproportionately impacted teenagers in the workforce, with the current rate of unemployment for those aged 16 to 19 at 14.3%, compared with 4% for those aged 20 and older. The American Hotel and Lodging Industry has predicted nearly four million people working in the hotel industry may lose their job. UBS predicts one-in-five restaurants could close due to the virus, with take-out and delivery orders not being enough to sustain business.22 Until the beginning of April, most states were not accepting unemployment claims from people who did not have traditional employers, such as gig workers, freelancers and the self-employed. However, the Pandemic Unemployment Assistance program recently passed by Congress extends much-needed benefits to these workers.23
Despite the surge in those needing medical treatment during this time, job security of those employed by the health care industry have also waned. A report from the Bureau of Labor and Statistics indicated the health care workforce lost 43,000 jobs in March 2020; primarily due to job losses in dental offices and private physician offices. While private practices and smaller health systems were the first to be negatively affected by COVID-19, some of the country’s largest health systems have also faced staggering financial losses – translating into significant job cuts and losses. The Hospital and Health Association of Pennsylvania (HAP) recently highlighted the financial challenge health systems are facing, stating that in March, "hospital operating margins dropped by an estimated $914 million compared to expectations.” The report added that Pennsylvania expects massive losses statewide for the upcoming financial quarter – roughly 4.5 billion dollars. Henry Ford Health System, located in Detroit, announced a mass furlough of nearly 3,000 employees across its six-hospital system, citing net losses of $234.5 million for the first quarter (a decrease of $354.9 million over the same period in 2019.) Johns Hopkins University (JHU), the umbrella organization which owns 50% of the Johns Hopkins Health System, has sought to implement various cost-cutting measures, including salary freezes for all staff and faculty, the suspension of retirement contributions and a sweeping organization-wide hiring freeze. The salaries of higher-level employees like the university president, provost and deans were also cut. Johns Hopkins Health System is the largest health system in Maryland and Johns Hopkins institutions are the largest non-government employer in that state. Before the pandemic, there were projections JHU would bring in $72 million in 2020 - now, it expects to lose $100 million. Since many of the nation’s hospitals’ usual stream of revenue (e.g. elective surgeries) have been postponed and/or cancelled, health care systems claim they cannot financially stay afloat without sacrificing employee jobs or cutting their pay.24 The Coronavirus Aid, Relief, and Economic Security (CARES) Act was signed into law on March 27.25 While $100 billion of the $2 trillion economic relief package earmarked for hospitals has helped, industry leaders have claimed it was not enough to account for the drastic losses they have endured; further, the House approved another relief bill that includes an additional $75 billion for hospitals.26
Job losses and financial instability have led to unprecedented housing insecurity in the United States. Mary Cunningham, a fellow at the Urban Institute, warned that shelter-in-place measures have created a situation in which low-income renters are now at high risk for eviction and homelessness, many of whom work in service industries hit exponentially hard by the pandemic shutdown. Cunningham added that the recent CARES Act, “didn’t do enough to address increases in housing insecurity for the nearly 11 million low-income renter households paying more than half their income toward rent before the pandemic. Low-income renters, especially those who lose employment during the crisis, will have a hard time paying back rent, and they could face housing situations that spiral out of control.” Supporting Cunningham’s claims, Avail, which is an online platform for landlords, conducted a survey of 2,775 landlords and 7,379 tenants; results indicated more than half of renters (53.5%) reported job losses due to measures enacted as a result of the COVID-19 pandemic.27 With 78% of Americans living paycheck-to-paycheck28, job cuts and losses will not only impact renters across the socioeconomic scope, but also homeowners seeking to make their next mortgage payment.
MATERIALS AND METHODS
Our exploratory, empirical research utilized an anonymous, online self-administered survey, that we designed and implemented on the Survey Monkey website. Questions were asked regarding respondents’ level of stress/anxiety/worry both before the pandemic and at current levels, their general concerns at this time as well as what impact the pandemic has had on their employment and health. Answers utilized both open-ended, scaled and multiple-choice format. The sample was obtained via online and social media methods, e.g. the Seattle Anxiety Specialists’ website, SAS Facebook page and Twitter accounts, resulting in a total of 1382 valid completions. Data was collected over a one-week period from April 16-22, 2020 and sought to collect data at one snapshot in time, during the peak of active Coronavirus cases in Seattle. We did not utilize the respondents within the Survey Monkey database as previous experience working in the private research sector has shown us that utilizing paid survey respondents can often result in rushed/inaccurate responses and lessen the validity of data. Additionally, by targeting respondents via SAS’ social media and online presence, there was a higher likelihood of obtaining respondents who suffer from increased stress/anxiety/worry than the general population, which was to assist Seattle Anxiety Specialists pinpoint what specific needs this cohort needs for assistance during this time of crisis.
To qualify for the study, respondents had to meet the following requirements:
live in Seattle and general surrounding area
minimum of 18 years old
Demographically, the sample is fairly balanced regarding respondents’ educational level and age, however, the sample yielded significantly greater females than any other gender – therefore data could not be cross-tabulated for that variable. Data was then cleaned to remove anyone who did not complete the survey after starting it and those who lived out of the target geographical area. Data analysis was conducted utilizing SPSS (IBM SPSS Statistics Subscription.)
RESULTS
Our results found both directional and significant evidence of psychological stressors occurring directly from the Coronavirus pandemic based on comparative data of the sample’s responses on a multitude of measures both prior to and following the outbreak.
Respondents indicated that money/finances as well as work issues/concerns were there primary worries before the COVID-19 pandemic. Following the outbreak of the virus, respondents indicated their concerns shifted to focus on their own health and safety as well as for their family. While there was a shift towards respondents expressing worry towards their own health, as well as the health of those they know, there was also a doubling in expression of care/concern towards the general population and various social issues (homelessness, environmental issues, inequality, etc.) suggesting that the pandemic has caused an increased sense of community and empathetic wanting to take care of ones’ neighbor.
Utilizing a six-point semantic differential scale, while respondents expressed greatest levels of stress/anxiety/worry regarding their own life in general, the greatest shift in concern occurred for: their friends (3.15); their own health and safety (3.05); and for their spouse/significant other (3.05). Respondents’ housing situation impacts current stress/anxiety/worry “high” levels reported in: 11.4% of homeowners; 30.6% of renters; 41.9% of those staying with family and 53.9% of those staying with friends.
Roughly 1/3 of the sample, 34.8%, has reported their employment situation has been negatively impacted by the pandemic. This shift is reflective of increased levels of stress/anxiety/worry regarding life in general, as well as respondents’ financial future.
Respondents reported nearly one-quarter became sick with some type of illness, and 3% were infected with the Coronavirus. Additionally, nearly 19% were unsure if they became ill, likely due to the complexity and sometimes vagueness of symptoms of COVID-19. 27% of respondents further noted that they knew a family member or friend who was infected with COVID-19 and 30% became ill with some other sickness.
For those who had gotten sick with Coronavirus or some other illness, the most frequent symptoms reported ranged from: muscle aches/pain; fatigue; fever; difficulty breathing; cough; nausea; chest pain; runny nose; memory issues and a fairly long duration of illness.
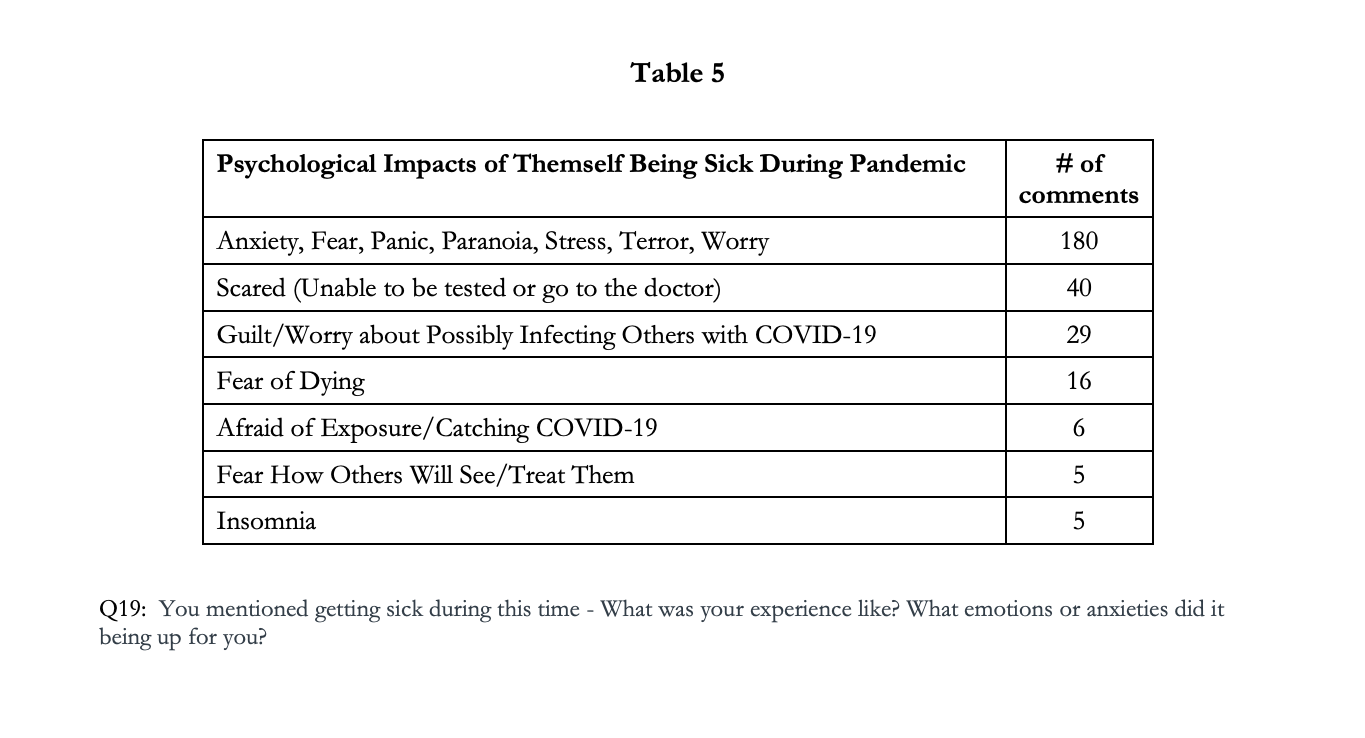
Whether they had Coronavirus or some other illness, the primary psychological impacts reported included those found in Table 5.
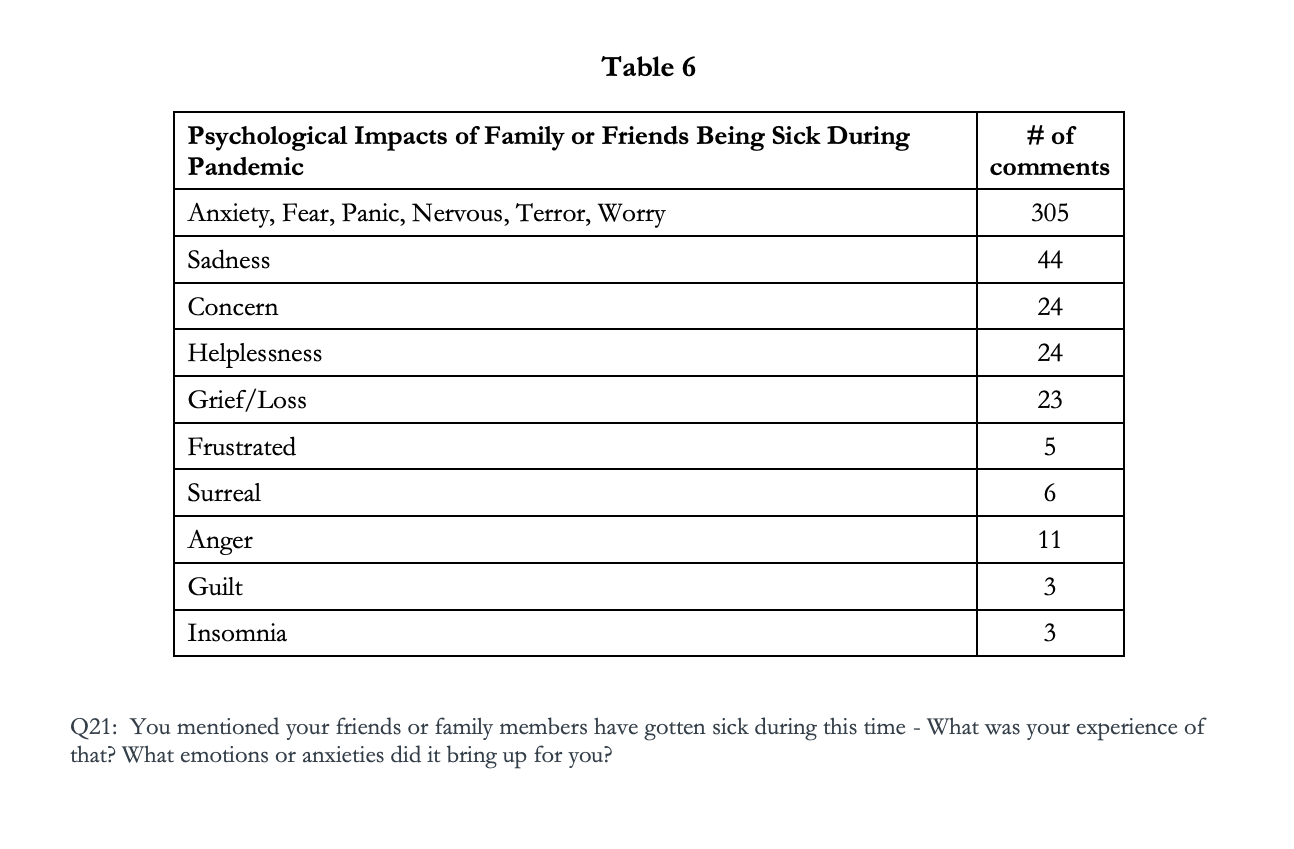
For those respondents commenting about negative psychological impacts they have endured when a friend and/or family member have gotten sick during the pandemic, their primary responses have been tabulated in Table 6. Note that several respondents indicated a lack of worry or concern due to the following reasons: finding out their friend/family were sick after they had recovered; the illness was minor; the friend/family member is not close to them and/or they were in good health and had a quick recovery.
Tables 7-8 denote significant differences in stress/anxiety/worry levels among the sample’s youngest and oldest age cohorts. Prior to the COVID-19 outbreak, respondents 65 and older reported significantly low levels of stress/anxiety/worry (51.9%), whereas only 15.5% of 18-24-year-olds reported low levels during that time. Additionally, following the pandemic, two-thirds of 18-24-year-olds indicated significantly highest levels of stress/anxiety/worry.
Levels of stress/anxiety/worry are correlated to respondents’ perception of the duration of the pandemic: those anticipating the pandemic to be “nearly over” indicate significantly lower levels of stress/anxiety/worry compared to the 51.9% of respondents who report high levels, and perceive the pandemic to be “ongoing and widespread a long time.”
Respondents aged 18-24 anticipate the COVID-19 pandemic to be “ongoing and widespread a long time” significantly more than the older cohorts.
While respondents are more likely to wear masks than gloves as personal protective equipment (PPE), their perception regarding the virus’ duration impacts how often they wear PPE. Those who perceive the pandemic to be “nearly over” never wear a mask 47.8% or gloves 69.6% of the time when out in public. Conversely, significantly more respondents wear PPE if they perceive the pandemic will be “ongoing and widespread a long time,” with 46.9% wearing a mask and 20% wearing gloves 75% of the time or any time they are in public (Tables 11-12).
There are polarizing correlations between age group and wearing PPE: those 65+ are significantly more-likely to wear masks and gloves in public compared to those 18-24 years-old (Tables 13-14).
Roughly 9-in-10 respondents report their quality of life has been impacted by the COVID-19 pandemic; nearly half of the sample indicating “significant” impacts. Of those 9-in-10 respondents, 19.5% of respondents have sought therapy at this time, with 64.3% saying they have not. (16.2% chose not to answer this question.) Those 18-24 reported the greatest impact on their quality of life (Table 17). Respondents 55+ were least-likely to seek out therapy during the pandemic (Table 18).
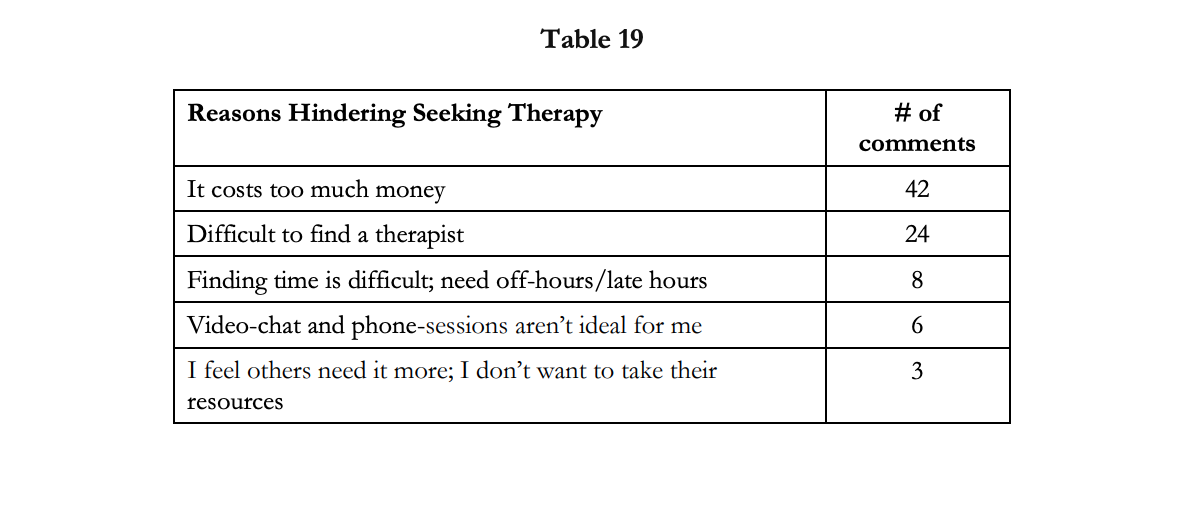
When prompted for any comments regarding whether they have sought therapy at this time, respondents reported financial aspects as well as difficulty finding a therapist as their main hinderances. Moreover, six respondents stated that they had reached out to therapists to begin counselling and never heard back from them.
As noted in previous research, low-income renters have been greatly-impacted during the pandemic and face housing instability. Our research has found that the pandemic has produced high levels of stress/anxiety/worry for home-owners as well as renters and those staying with family and friends. Mindful of low base-sizes, those staying with friends during the pandemic report highest levels of stress/anxiety and worry at this time.
DISCUSSION
Our results highlighted the importance of utilizing both open-ended and closed-ended answer choices in a survey or when speaking with a patient in therapy. Although respondents indicated that money/finances and their work/retirement and/or school situation were of lessened worry to them during the pandemic than they previously were, these variables were reported to have the greatest shift in stress/anxiety/worry among respondents. While respondents were less-likely to voice as much concern for money/finances and their work/school situations in a pandemic situation, the stress and anxiety for these matters were latently significant, impactful in their lives and require addressing to ease stress during this time.
Tables 7-8 stress/anxiety/worry among age groups: while those 65+ are in the highest-risk group regarding COVID-19, this cohort is the most-likely to be retired and thus financially secure in the sample. While those 18-24 face the lowest health-burden of the pandemic, they are financially the most negatively-impacted regarding finding/maintaining secure employment, which is reflected in this cohort’s significant levels of stress/anxiety/worry. The highest perception that the pandemic will be ongoing and widespread is also likely leading to 18-24-year-olds enduring the greatest level of stress/anxiety/worry at this time (Table 10). Likely due to the susceptibility and health risks to those 65+, this group is significantly most likely to use PPE in public; those least-likely to wear PPE comprise the 18-24-year-old cohort, who are medically least-likely to face serious health consequences if infected with Coronavirus (Tables 13-24).
Roughly 9-in-10 respondents report their quality of life has been impacted by the COVID-19 pandemic; nearly half of the sample indicating “significant” impacts. Of those 9-in-10 respondents, 19.5% of respondents have sought therapy at this time, with 64.3% saying they have not. (16.2% chose not to answer this question.) Those 18-24 reported the greatest impact on their quality of life (Table 17). Respondents 55+ were least-likely to seek out therapy during the pandemic (Table 18).
When prompted for any comments regarding whether they have sought therapy at this time (Table 19), respondents reported the financial cost as the biggest hinderance, particularly during this time of financial uncertainty and/or with many earning less than what they previously have (e.g. 35% of the sample reported being laid-off, furloughed, their business suffering, etc.)
The second most-prominent reason for not attending therapy during this time of acute stress is reported to be difficulty in finding a therapist and not knowing where or how to seek one out. Further, some respondents added that they would need an appointment other than standard Monday-Friday, 9:00am-5:00pm and finding a therapist with hours to accommodate their schedule has proven difficult. Others reported reaching out to therapists, only to not hear back or be contacted for an appointment. Further, during this time of decreased services and stay-at-home ordinances, six respondents expressed issues with video-chat and/or phone sessions and said they would do better with in-person therapy sessions. Lastly, three respondents were altruistic in their reasoning for delaying attending therapy and cited not wanting to take away limited resources from those who may need counseling more than themselves.
To provide the greatest assistance to those significantly psychologically impacted by the COVID-19 pandemic, therapists and counseling services should enact the following:
advertise their practice’s availability and acceptance of new patients;
offer appointments with varied hours, such as early morning, late night and weekends;
offer in-person appointments in a safe and clean environment;
provide low-cost counseling options, if possible;
and provide free online resources and guides to assist with psychological stressors and trauma during a pandemic.
Tables 5-6 support the findings of the CDC regarding common signs of distress during the pandemic. While our research finds commonalities with the list the CDC warned to be mindful of, our sample noted several other manifestations of distress at this time. Healthcare providers should therefore be cognizant to address these issues/ailments in patients during the pandemic.
REFERENCES
“2019 Novel Coronavirus Outbreak (COVID-19),” Washington State Department of Health (2020) www.doh.wa.gov/emergencies/coronavirus
Ibid.
“Coronavirus Disease 2019 (COVID-19): Situation Summary,” Centers for Disease Control and Prevention (2020) www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html
Ibid.
Ibid.
Ibid.
“Data Models on COVID-19 Deaths in Washington Offer Hope, Challenges,” KOMO News (2020) https://komonews.com/news/coronavirus/new-models-show-social-distancing-making-positive-impact-in-washington-state
“COVID-19 Projections: Washington State,” IHME (2020) https://covid19.healthdata.org/united-states-of-america/washington
“2019 Novel Coronavirus Outbreak (COVID-19),” (2020)
“Coronavirus Disease 2019 (COVID-19): Situation Summary,” (2020)
“2019 Novel Coronavirus Outbreak (COVID-19),” (2020)
“Coronavirus Disease 2019 (COVID-19): Stress & Coping,” Centers for Disease Control and Prevention (2020) https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html#risk
Ibid.
Ibid.
“Emergency Preparedness and Response: Taking Care of Your Emotional Health,” Centers for Disease Control and Prevention (2020) https://emergency.cdc.gov/coping/selfcare.asp
“COVID-19: Roughly 1 in 10 Workers Have Lost Their Jobs in the Past 3 Weeks,” MarketPlace (2020) https://www.marketplace.org/2020/04/09/covid-19-unemployment-claims-6-6-million/
“Nearly 60% of People Who Have Lost Their Jobs Due to the Coronavirus Pandemic are Women, According to Report,” Business Insider (2020) https://www.businessinsider.com/coronavirus-unemployment-women-60-percent-2020-4
“COVID-19: Roughly 1 in 10 Workers Have Lost Their Jobs in the Past 3 Weeks,” (2020)
“Home Page,” Washington State Employment Security Department (2020) www.esd.wa.gov
“Employment,” Washington State Employment Security Department (2020) https://www.esd.wa.gov/unemployment/help
“Unemployment Insurance Relief During COVID-19 Outbreak,” U.S. Department of Labor (2020) https://www.dol.gov/coronavirus/unemployment-insurance
“Nearly 60% of People Who Have Lost Their Jobs Due to the Coronavirus Pandemic are Women, According to Report,” (2020)
“COVID-19: Roughly 1 in 10 Workers Have Lost Their Jobs in the Past 3 Weeks,” (2020)
“Even Nation’s Largest Health Systems Laying Off Health Care Workers Amid COVID Pandemic,” ABC News (2020) https://abcnews.go.com/Health/coronavirus-victim-americas-largest-health-systems/story?id=70317683
“Unemployment Insurance Relief During COVID-19 Outbreak,” (2020)
“Even Nation’s Largest Health Systems Laying Off Health Care Workers Amid COVID Pandemic,” (2020)
“More Than Half of Renters Say They Lost Jobs Due to Coronavirus,” MarketWatch (2020) https://www.marketwatch.com/story/they-could-face-housing-situations-that-spiral-out-of-control-more-than-half-of-renters-say-they-lost-their-jobs-due-to-covid-19-2020-04-09
“78% of Workers Live Paycheck to Paycheck,” Forbes (2020) https://www.forbes.com/sites/zackfriedman/2019/01/11/live-paycheck-to-paycheck-government-shutdown/#26f5b64d4f10